A single drug doesn’t cure cancer. Neither does one machine or one test result. What has changed — deeply — is how the body gets involved. Immunotherapy doesn’t just fight cancer. It shifts the battlefield to inside the immune system itself. That approach isn’t new, but it’s finally catching up with what science can do. And not everyone agrees on where it works best.
Some tumors respond not because they’re weak, but because the immune system was waiting
Cancer doesn’t always outsmart the body. Sometimes, it slips through quietly. The immune system notices, but doesn’t respond. Immunotherapy attempts to unlock that silence. Certain tumors have strong immune signals already. Melanoma, for example, shows markers that attract T-cells. The drug doesn’t kill — it tells the immune system to attack. But without that invitation, the system stays passive. That’s why immunotherapy works better in some cancers than others.
Checkpoint inhibitors don’t push harder — they remove what’s holding the immune system back
Your immune system uses brakes, not just gas pedals. That’s how it avoids attacking itself. Cancer often takes advantage of those brakes. Checkpoint inhibitors lift that control. Drugs like pembrolizumab block the PD-1 signal. Once that’s off, immune cells regain their strength. But that doesn’t mean chaos. Not every response is equal. Some patients experience inflammation. Others improve dramatically. It depends on context, not just drug.
Results don’t follow timelines, and success may take longer than expected
Chemotherapy often shows progress within weeks. Immunotherapy moves differently. Tumors may swell first — then shrink. Or remain unchanged, then vanish. This frustrates patients and doctors alike. Imaging may mislead. Waiting becomes part of the strategy. In Dubai clinics, this leads to extra scans. In Istanbul hospitals, oncologists discuss “pseudo-progression.” It’s a real phenomenon. But it demands patience.
Side effects are less visible but often harder to predict
Immunotherapy isn’t free from toxicity. It simply creates different risks. Some patients develop colitis. Others develop thyroid problems. Skin reactions appear without warning. These side effects don’t follow typical dosage patterns. They emerge weeks later. In some cases, long after treatment stops. The immune system keeps acting — even when the drug is gone. That’s what makes it both powerful and unpredictable.
Combination therapies are increasing, but not all combinations are helpful
One drug rarely does enough. Researchers try combining immunotherapy with chemotherapy or radiation. Sometimes, this boosts results. Other times, it compounds toxicity. Clinical trials test dozens of combinations. But real-world patients don’t always match those profiles. In Turkey, patients often receive immunotherapy after other options fail. In the UAE, private insurers limit access to combo treatments. That changes what’s available — and when.
Some tumors adapt quickly, forcing the immune system to re-learn recognition
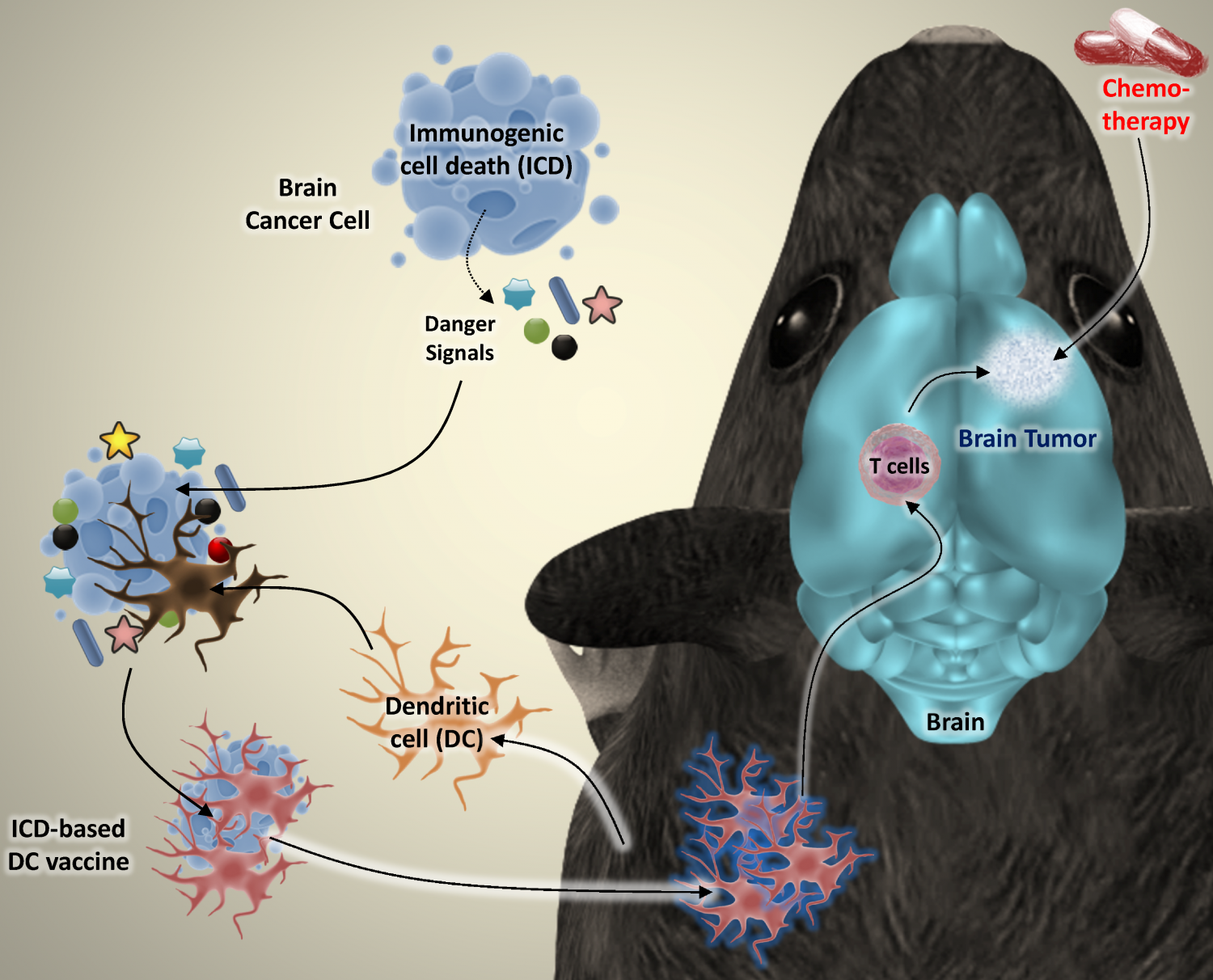
Cancer evolves. Even within the same body. Some cells develop resistance after initial response. That resistance doesn’t always mean the drug failed. It means the tumor changed its face. Immune memory must catch up. This has led to interest in vaccine-style boosters. Not traditional vaccines, but personalized ones — built from the tumor itself. That work is still in trials, but promising.
Success depends on biomarkers, but we still don’t agree which ones matter most
PD-L1 expression predicts success — sometimes. Tumor mutational burden helps — maybe. Microsatellite instability seems useful — in some cancers. But none are universal. One patient may respond without any biomarkers. Another may have them all — and fail. This makes selection tricky. Dubai’s large oncology centers now run full molecular profiling. Istanbul’s research hospitals prioritize biopsies for gene panels. But access varies by location and budget.
Financial cost shapes access more than clinical factors in many regions
These therapies aren’t cheap. One course may cost tens of thousands of dollars. Insurance doesn’t always cover newer agents. Governments subsidize some cancers but not all. That divides patients by system, not need. In the Gulf region, expats without full coverage face denial. In Turkey, state hospitals offer limited access based on protocol tiers. The science moves faster than the systems can adapt.
Immunotherapy trials often exclude the very patients who need options most
Clinical trials require stability. But real patients are rarely stable. Those with multiple conditions often get excluded. Elderly patients, pregnant women, or those with prior autoimmune disease — all left out. That creates a gap between evidence and reality. Some doctors still prescribe off-label. Others hesitate. Patients sense the uncertainty. And yet, it’s often their only chance.
Patients must learn the language of their own biology to stay informed
Terms like “neoantigens,” “immune profiling,” and “tumor microenvironment” matter. Not for curiosity — but for decisions. Doctors explain what they can. But time is short. Patients who ask specific questions get better answers. In Dubai, multilingual staff helps. In Turkey, support groups bridge the information gap. Still, most people search online. Knowing what to ignore becomes its own skill.
Oncologists don’t always agree on when to stop treatment
When imaging shows stable disease, what does it mean? Is that success or stagnation? Should the patient continue — or rest? Immunotherapy blurs that line. Some doctors continue beyond response. Others stop early to avoid side effects. There’s no universal rule. Only context. In major cancer centers, tumor boards debate each case. But in solo clinics, decisions are personal — and harder.
Remission may not look like absence — but like control
Immunotherapy doesn’t always erase disease. Sometimes it contains it. Keeps it still. Shrinks the reach. That can feel like a half-win. But for some cancers, that’s the goal. Turning aggressive growth into silent presence. If a tumor stays quiet for years, that’s success. Even if it doesn’t disappear. This changes how remission is defined.
Time matters less than direction when tracking response
Doctors don’t just watch the tumor size. They watch stability. Bloodwork, breathing, fatigue — they track trends. Up or down. Fast or slow. Movement matters more than shape. This helps guide next steps. Immunotherapy isn’t about perfect curves. It’s about the slope. And sometimes, the flattest line is the biggest relief.
The future of immunotherapy depends on what the body already knows
The immune system isn’t a blank slate. It remembers, forgets, reacts, and adapts. Future treatments aim to harness that memory. To teach the system in layers. Cancer vaccines, T-cell engineering, dendritic cell reprogramming — these aren’t science fiction. They’re on the table. But success still depends on timing. On early detection. On access. On staying one step ahead — not just with machines, but with understanding.
Source: Best Oncologist in Dubai / Best Oncologist in Abu Dhabi