The immune system remembers everything. Not just colds or wounds, but patterns, fragments, intruders it didn’t understand. For decades, cancer escaped this memory. Immunotherapy changes the script. It doesn’t replace chemotherapy. It doesn’t eliminate surgery. It rewrites the dialogue between disease and defense. And that rewrite isn’t finished.
It doesn’t work by killing the tumor directly
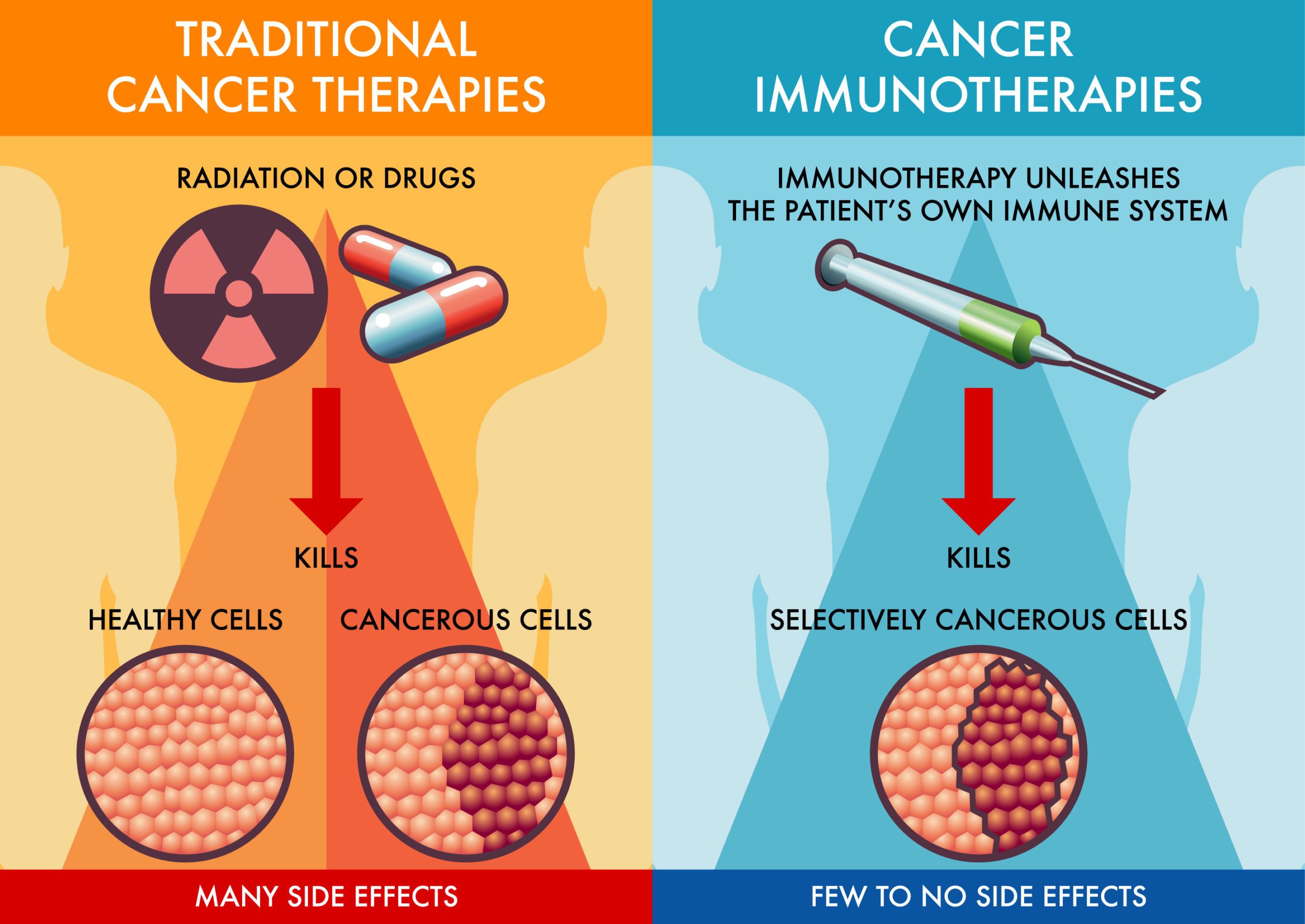
Traditional cancer treatments target cells. Immunotherapy does something else. It teaches the body to do the work. That shift isn’t aggressive. It’s precise. Immune cells, when activated, can find targets chemotherapy overlooks. They move differently. They recognize. They adjust. But not always. And not everywhere.
Some tumors respond only when the immune system was already prepared
There are tumors the immune system already recognizes, but only barely. Melanoma is one. Lung cancer too. In these cases, the immune system waits for permission. Checkpoint inhibitors grant that. They remove the handbrake. But if recognition never existed, the system stays quiet. Immunotherapy works best when that whisper is already present.
Checkpoint inhibitors lift the immune system’s internal brakes
The immune system is careful. It knows not to attack itself. Tumors exploit that. They mimic safe cells. Checkpoint inhibitors block that mimicry. PD-1, CTLA-4 — names that mean pause. The drugs block them. The pause ends. The attack begins. But the result depends on many things. Not all brakes are equal.
Progress doesn’t always look like progress on a scan
After treatment, a scan might show swelling. Not growth. Just the immune system showing up. It causes inflammation. That looks like worsening. But it isn’t always. Doctors call it pseudoprogression. Sometimes the real shrinkage comes weeks later. Sometimes never. The scan can’t always tell you when to hope.
Side effects appear far from where the cancer began
Because this isn’t chemotherapy, the side effects come from somewhere else. They come from the immune system’s reach. It might target the colon. Or the thyroid. Or the skin. These aren’t accidents. They’re signs the system is awake. But awake doesn’t mean accurate. Sometimes, it overreacts. Sometimes, it lingers too long.
Sometimes nothing happens until something shifts suddenly
Immunotherapy often moves silently. No change. No symptoms. Then, suddenly, a drop in tumor markers. A scan showing clearance. Or the reverse. Nothing for months. Then new growth. This unpredictability makes planning difficult. But it also means patience matters. Not all movement is fast. Some is quiet, and then sudden.
Combination treatment isn’t always about strength — it’s about timing
Immunotherapy rarely works alone. It combines with other therapies — but not randomly. Timing matters. Radiation before immunotherapy might prime the immune system. Chemotherapy might lower suppression. But bad timing causes exhaustion. Not synergy. Doctors argue over sequencing. Trials continue. Patients wait.
Every patient’s immune system tells a different story
Biomarkers try to predict who will respond. PD-L1 expression, tumor mutation burden, mismatch repair status. They help. But they aren’t rules. Some patients respond with no markers. Some markers mean nothing. The immune system doesn’t follow charts. It follows memory, context, confusion. Tests guide, not guarantee.
Tumor location changes how the immune system behaves
A tumor in the brain responds differently than one in the liver. The environment matters. Some tissues suppress immune entry. Others attract it. Blood vessels, chemical signals, previous infections — all influence response. A drug that works in lung cancer might fail in colon cancer. Not because of genetics. Because of geography.
Cost changes what doctors can offer and when
These treatments are expensive. Some cost more than $10,000 per dose. Insurance doesn’t always pay. Public systems ration. Private clinics depend on policy. In Turkey, access depends on protocol codes. In Dubai, many expats face policy caps. Patients ask, “Is there a cheaper option?” Sometimes there isn’t.
Autoimmunity may appear even after stopping the drug
You finish treatment. Months pass. Then your joints ache. Your skin reacts. Your thyroid slows. This happens. The immune system sometimes stays alert long after the drug leaves. It acts as if the threat remains. Doctors manage this with steroids, hormone therapy, or monitoring. But it surprises many patients.
The tumor isn’t the only thing changing — the immune system changes too
As cancer adapts, so does immunity. The immune response may grow stronger or more confused. It may begin recognizing new parts of the tumor. Or lose interest. That’s why some patients respond later than expected. The immune system finds a new target. Or finally understands an old one.
Cell therapy personalizes the immune system for a single patient
Some treatments go deeper. They take immune cells out, reprogram them, and return them. CAR-T therapy does this. So do TIL therapies. These are complex. They take time, money, precision. But they aim at customization. Your cancer. Your immune cells. Matched like a lock and key. But not everyone qualifies.
Not all responses are visible — some are simply a pause
In some cases, the cancer stops growing. It doesn’t shrink. But it doesn’t spread either. This stability may last months. Even years. For some patients, that’s enough. Living with cancer, not dying from it. This changes how we talk about remission. It’s not always about disappearance. Sometimes it’s about stillness.
Doctors debate how long to continue after stability appears
When should treatment stop? After a year? Two? If scans stay stable? There’s no consensus. Some stop early to avoid side effects. Others continue to maintain the effect. Studies offer guidance. But each case unfolds differently. Doctors decide based on risk, age, tolerance, preference. The answer shifts with the patient.
The most powerful tools are often invisible in scans and labs
Fatigue that lifts. Appetite returning. Pain fading. These aren’t always captured in reports. But they matter. A patient says, “I feel clearer.” That might come before any scan does. Immunotherapy’s impact sometimes appears in words, not numbers. Listening becomes diagnostic. Observing becomes part of treatment.